Latent Autoimmune Diabetes of Adults (LADA) is another name for Type 1.5 Diabetes (T1.5D). Some specialists in the field believe that LADA is a distinct kind of diabetes, while others believe that it is a slowly developing variant of Type 1 Diabetes (T1D).
While T1D is typically diagnosed in children and younger people, LADA or T1.5D is occasionally confused with T1D in adults over the age of thirty. Type 2 Diabetes (T2D) and T1.5D are frequently seen together; in fact, up to 25% of people with T1.5D also have T2D-like traits.1. It’s sometimes referred to as “double diabetes.”
All T1.5D patients eventually become insulin-dependent and are at a very high risk of developing an insulin need within months or years (up to six years) of receiving their initial diagnosis. People with T1D, on the other hand, typically require insulin within days or weeks of diagnosis.2 Insulin therapy is very uncommon for people with T2D. Although it is not generally agreed upon, the current guidelines are to treat people with T1.5D with insulin right away (see below).
The Reasons Behind T1.5D
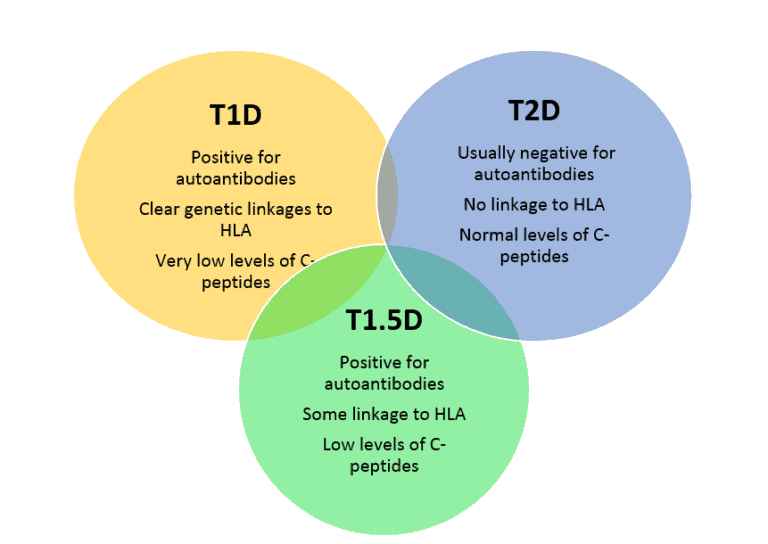
As with other types of diabetes, the fundamental cause(s) of T1.5D remain unknown to us. It is evident that, similar to Type 1 Diabetes, the immune system has become “confused” and is acting against the pancreatic beta cells, which are the source of the insulin required to regulate blood sugar levels. There are autoimmune components to Types 1, 1.5, and 2 diabetes, as well as some overlap in the types of antibodies formed. Anti-GAD, or glutamic acid decarboxylase, antibodies are present in both T1D and T1.5D. Similar to those with T1D, most people with T1.5D are overweight or obese, whereas most people with T2D are not.
Environmental Susceptibility and Genetics
Although there does not seem to be as strong of a correlation, individuals with T1.5D share many of the same genetic susceptibilities as those with T1D, including the HLA-DR and DQ families (haplotypes).3. additional genes, many of which are involved in immune system functions, are linked to both T1D and T1.5D. These genes include those linked to T cell activation (CTLA4, PTPN22, IL2RA), as well as a variety of additional genes. Since T1.5D patients are typically identified later in life, environmental susceptibilities are hypothesized but not fully understood at this time.4
Symptoms
T1.5D symptoms include increased frequency of thirst, increased frequency of urine, and inadvertent weight loss, which are comparable to those of other kinds of diabetes. Additional symptoms like weariness or blurred vision could also appear. Usually, T1.5D is first diagnosed as T2D and is only taken into consideration when blood sugar-controlling drugs have failed to control the condition. These medications are most frequently sulfonylureas, which are covered in the section below, but metformin can also cause treatment failure. When these popular anti-diabetic drugs don’t work, more tests are carried out to check for antibodies and low levels of C-peptide, a normal material that’s used as a biomarker for both T1D and T1.5D.
Identification
Numerous T1D symptoms and some antibodies are shared by those with T1.5D. On the other hand, people with T1.5D often only have one of the following antibodies, but people with T1D may have two or more of them:
- Anti-Islet cell antibodies Antigens (ICA-resistant)
- The chemical sequences known as antigens are what cause antibodies to develop.
- Antibodies to glutamic acid decarboxylase (also known as GADAs or anti-GAD antibodies).
- In T1.5D, these are the most prevalent.
- Tyrosine phosphatase protein antibodies (IA-2s)
- Insulin-specific antibodies
Generally speaking, beta-cell breakdown increases with elevated levels of self-antibodies (autoantibodies), and an individual with T1.5D may require insulin replacement therapy sooner. T1.5D should be suspected in anyone with diabetic symptoms AND another autoimmune disease, such as Hashimoto’s thyroiditis, rheumatoid arthritis, celiac disease, lupus, or any other autoimmune disease, as one autoimmune problem raises the risk of other autoimmune disorders.5.
The following criteria are used by the Immunology of Diabetes Society to diagnose T1.5D patients:4
- older than thirty years
- Positive for at least one of the four antibodies that T1D patients frequently have
- not needed insulin therapy over the first six months following diagnosis.
Comparing people with T1.5D to those with T2D, they are similar in terms of insulin resistance and blood sugar regulation.
Additionally, T1.5D exhibits a comparatively low level of the C-peptide biomarker, which is increasingly being used to differentiate T1.5D from T2D.6 C-peptide levels are very low in T1D patients, low in T1.5D patients, and normal in T2D patients.
In general, there are several reasons why the diagnosis of T1.5D may be challenging:
- There is considerable overlap in symptoms and test data, and opinions about the differences between T1D, T1.5D, and T2D are not widely held.
- T1.5D is a relatively recently identified illness, and nothing is known about its traits or recommended course of therapy.
Handling
Insulin is the “treatment of choice” for T1.5D and should be started as soon as feasible, despite the fact that current guidelines recommend an insulin-free period of six months. therapy for T1.5D is identical to that for T1D.7. For those who are overweight or obese, calorie restriction combined with diet and exercise can be helpful.
It is critical to make the right diagnosis because there are some worries about some blood sugar-lowering medications. Sulfonylureas like glimepiride, glyburide, and glipizide may need to be avoided because they stimulate the pancreatic beta cells, which may lead to increased antibody destruction of these cells.8,9 If necessary, metformin can be administered with caution. At least some data suggest that medications like exanatide and sitagliptin may be the most effective at controlling blood sugar in individuals with T1.5D.
Issues related to T1.5D
T1.5D patients are more likely to experience heart disease, stroke, and microvascular consequences like eyesight, nerve, and kidney damage, just like individuals with other types of diabetes. The earlier insulin treatment is started, the lower these hazards seem to be.
Citations
- http://diabetes.diabetesjournals.org/content/54/suppl_2/S68.full
- http://www.clinicaladvisor.com/diabetes-resource-center/diagnosis-and-treatment-of-latent-autoimmune-diabetes-in-adults-still-evolving/article/203578/
- http://www.idf.org/sites/default/files/attachments/article_5_en.pdf
- http://diabetes.diabetesjournals.org/content/54/suppl_2/S62.full.pdf+html
- http://www.aafp.org/afp/2010/0401/p843.html
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3354922/#ref10
- http://diabetes.diabetesjournals.org/content/54/suppl_2/S68.full
- Näntö-Salonen K, et al. Lancet 2008
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3354922/
